Introduction
Opioid prescribing has been in the spotlight since the opioid epidemic was declared in the United States. The correct prescription of these medicines requires a good understanding of their pharmacodynamics and pharmacokinetics (1), training in pain pathology and knowledge about possible therapeutic alternatives that can replace or being combined with these drugs in a multimodal strategy (2). If a national training plan is to be established for doctors on the management of opioid drugs, it is essential to know which specialties concentrate the most part of these medicines’ prescriptions and on which indications they are being prescribed the most.
Methodology
Quantitative data from the study of medical prescriptions provided by IQVIATM have been analyzed. These data come from IQVIA’s databases and collect information on the prescriptions of medicines made in Spain during the period 2019 and 2020. The data was collected in a sample of pharmacies throughout the national territory and then extrapolated at national level. The data correspond to MAT (Mobile Annual Rate) of June 2019 and June 2020. They include information about the number of prescriptions performed by each medical specialty, per molecule, and per diagnosis. 21,724 data was obtained. Once the data was collected and organized, several pivot tables were made using Microsoft Excel software. With these pivot tables, several crossed analyses were made to obtain: the number of prescriptions per molecule and specialty, the number of prescriptions per molecule and indication, the number of prescriptions per specialty and molecule and, finally, the number of prescriptions per diagnosis and molecule. Since diagnostic information was very extensive, some clusters were performed depending on the clinical scope. Prescriptions by type of formulation for each opioid molecule were also analyzed.
Results
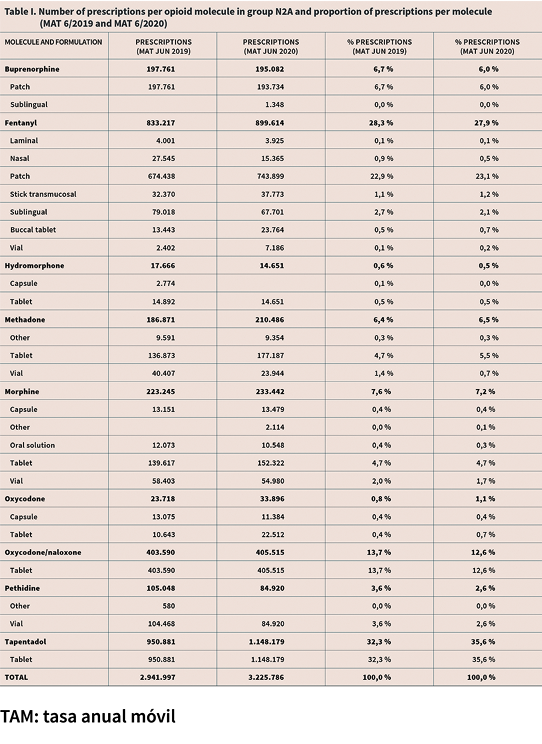
Total prescriptions per molecule
The MAT at June 2020 shows that 3.2 million opioid prescriptions of the N2A group had been performed in Spain, corresponding to the step III opioids. 36 % of them were tapentadol, which was the most prescribed molecule in this group, followed by fentanyl with 28 % and oxycodone-naloxone with 13 % (Table I).
In the case of fentanyl, 81 % of the prescriptions corresponded to the patch formulation while the remaining 19 % corresponded to immediate release formulations, being the sublingual one the most frequently prescribed within the latter subgroup.
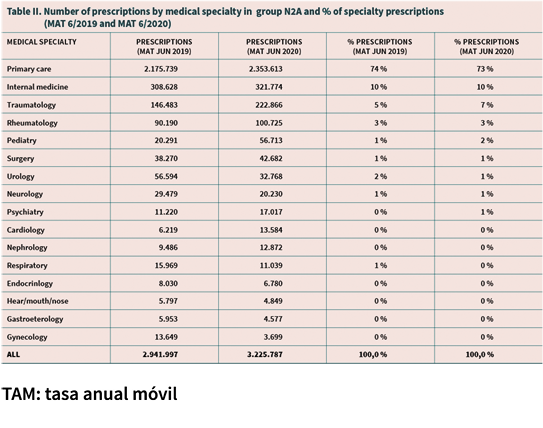
Prescriptions by medical specialty
73 % of the prescriptions had been made by the primary care physician becoming the largest prescriber of the N2A group in Spain. The internal medicine specialist was the second with 10 % of all prescriptions while traumatology specialists (7 %) rheumatology (3 %) were the third and fourth respectively. The rest of specialties together represent only 7% as a whole (Table II).
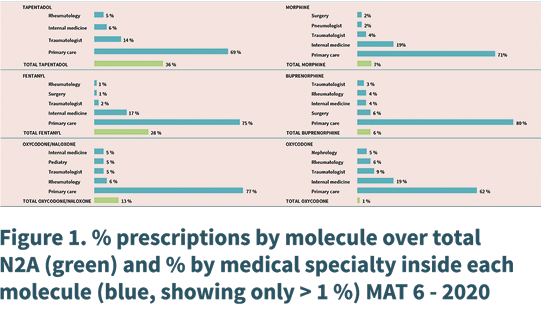
Prescriptions per medical specialty for each opioid molecule
70 % of tapentadol’s prescriptions had been performed by primary care while 14 % were performed by the traumatologist, 7 % by internal medicine and 4 % by rheumatologist. As for fentanyl, 75 % of its prescriptions were made by AP and 17 % by internal medicine, being the rest of the specialties much more minority. As for oxycodone-naloxone, 78 % were from primary care doctors and 8 % were made by rheumatologists (the highest percentage this specialty has across all the molecules). Pediatricians made the 5 % of the total prescriptions of oxycodone-naloxone. In relation to buprenorphine, surgeons made the 5 % of its total prescriptions. Finally, in oxycodone alone we could highlight as differential that a 5 % of its prescriptions were made by nephrologist (Figure 1).
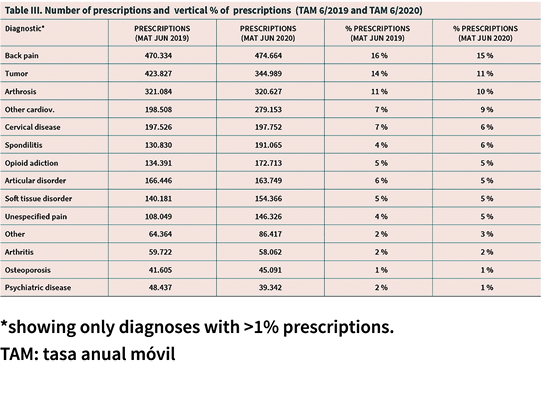
Diagnostic prescriptions
As for the use of opioids by diagnosis the two most relevant are back pain (15 %), cancer (11 %) osteoarthritis (10 %). There is a large dispersion of diagnoses in which these drugs are used in pathologies in all clinical areas (Table III).
Prescriptions by clinical area
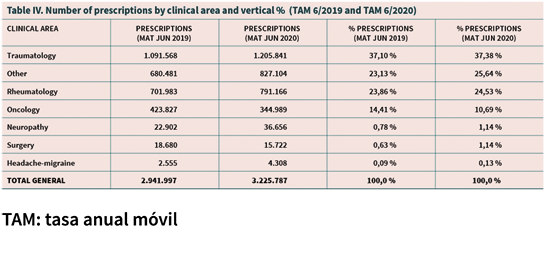
After performing a grouping of diagnoses by clinical areas, we obtained that the areas of highest concentration of opioid prescriptions were: traumatology with 38 % of prescriptions, rheumatology with 26 % and oncology with 11 %. These 3 clinical areas concentrate 73 % of total opioid prescriptions (TAM June 2020) with figures similar to those for the same period in 2019 (75 %) (Table IV).
Prescriptions by molecule and clinical area
76 % of tapentadol prescriptions were made in traumatology or rheumatology diagnoses while only 3 % were made in oncology.
Regarding fentanyl, the trauma-rheumatology area concentrated 46 % of its prescriptions and oncology the 22 %.
In the case of oxycodone-naloxone, 77 % of its prescriptions were in indications of trauma-rheumatology and 4 % in oncology while oxycodone was used in trauma-rheumatism by 35 %, 6 % in oncology and in 4 % in surgery. Morphine was the relatively most commonly used opioid in oncology with 34 % of its prescriptions in this clinical area.
Discussion
Our study quantified 3.2 million annual prescriptions by TAM June 2020, which would equate to a rate of 0.06 prescriptions per capita per year, which is a very low level when compared to the US data in 2012, which was 289 million prescriptions in total equivalent to a ratio of 0.92 requirements per capita per year (3).
This study shows that the primary care physician is the one who concentrates the vast majority of opioid prescriptions in Spain (73 % in 2020) while in a similar US study in 2012 this medical group only performed 18 % of the total opioid prescriptions (3). This was confirmed in another 2014 MEDICAID data-based study (4) where primary care doctors performed 23 % of prescriptions. This difference in the role of primary care doctors may explain, at least in part, the closer opioid patient monitoring in Spain to the United States
In our study we do not have the data on the percentage of primary care prescriptions which were initiated by the primary doctor’s own decision and which ones were a repetition of a prescription for a treatment decided by a specialist and, therefore, it becomes difficult to know the actual level of initiations of opioid treatments that are performed in primary care setting. What we can conclude is that the follow-up and monitoring of patients in treatment with these drugs lies primarily in the primary care. European guides (EFP) (1) and recommendations of various scientific actors from 1986 (Portenoy) (5) to the most recent ones (Montreal declaration (6) or V vital sign [7,8]) highlight the importance of good monitoring of the patient in opioid treatment and the need for doctors who initiate or follow opioid treatments to be properly trained. With the results of this study, it seems clear that training on opioid management to primary care physician should be a priority for health systems in Europe. This conclusion can also extend to the other specialties that handle these drugs frequently, especially to doctors of internal medicine, traumatology and rheumatology that would be the following in importance in terms of volume of opioid prescriptions in Spain.
As for the most prescribed molecules, there are 3 that sum the 77 % of total prescriptions (tapentadol, fentanyl and oxycodone-naloxone). It is important to note that 81 % of total fentanyl correspond to the patch fentanyl that is indicated for the treatment of chronic pain while only 19 % of fentanyl (5 % of all opioid prescriptions) correspond to the immediate release fentanyl.
With regard to the specialists who prescribed each molecule, in all cases most prescriptions are maintained from the GP (general practitioner), however, there are some relevant differences, such as the relative importance of traumatologists in tapentadol, rheumatologists in oxycodone-naloxone and tapentadol, surgery in buprenorphine and endocrinology in hydromorphone. This fact may make us think that also these specialties should be included in the training plan mentioned above. This is a differential fact with respect, for example, to prescription dynamics detected in the United States, where a significant portion of the prescriptions are performed by dentists, physiotherapists or nurses (3). A 2015 study published by Levy et al (3), which also used IQVIA data referred to the United States, found that 32 million opioid prescriptions in 2012 had been performed by nurses or physician assistants, 18.5 million were performed by dentists, and only 14.5 million were performed by pain specialists.
The 2014 MEDICAID data-based study (4) identified that dentists in the United States were 3.5 times more likely than GPs to prescribe opioids, and traumatologists were 7 times more likely to prescribe these drugs than primary care doctors. The role of dentists in the United States as intensive opioid prescribers should be analyzed as in the mentioned study (4) a 30 % of total opioid prescriptions in chronic pain and 26 % of total prescriptions for treating arthritis had been performed by a dentist. These indications, a priori, would be outside the scope of a dentist’s clinical practice and could also explain, in part at least, the over-prescription detected in that country. In fact, a 2017 study (9) conducted a correlation analysis of the factors associated with increased opioid use in several counties in the United States, finding several characteristics that were associated with a higher level of opioid prescription, being the highest number of dentists per 100,000 inhabitants one of those factors.
Finally, in terms of the use of opioids by diagnosis and by clinical area, it becomes clear that the indications of trauma-rheumatology are the ones that bring together the most prescriptions, constituting 64 % of the total. Oncology indications represent only 11 % of all opioid prescriptions so, although they may seem to represent in the past the main indication of opioid painkillers (when only their use was indicated in cancer patients who “could count their life in weeks”), they are a minority of the current use of these drugs in our country.
REFERENCES
1. O’Brien T, Christrup LL, Drewes AM, Fallon MT, Kress HG, McQuay HJ, et al. European Pain Federation position paper on appropriate opioid use in chronic pain management. Eur J Pain. 2017;21(1):3-19. DOI: 10.1002/ejp.970.
2. Chou R, Gordon DB, De Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-57. DOI: 10.1016/j.jpain.2015.12.008.
3. Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic-prescribing rates by specialty, U.S., 2007-2012. Am J Prev Med. 2015;49(3):409-13. DOI: 10.1016/j.amepre.2015.02.020.
4. Ringwalt C, Gugelmann H, Garrettson M, Dasgupta N, Chung AE, Proescholdbell SK, et al. Differential prescribing of opioid analgesics according to physician specialty for Medicaid patients with chronic noncancer pain diagnoses. Pain Res Manag. 2014;19(4):179-85. DOI: 10.1155/2014/857952.
5. Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: report of 38 cases. Pain. 1986;25(2):171-86. DOI: 10.1016/0304-3959(86)90091-6.
6. Declaration of Montreal. IASP-PAIN.ORG. 2010. Disponible en: https://www.iasp-pain.org/DeclarationofMontreal [citado 10 de octubre de 2020].
7. Morone NE, Weiner DK. Pain as the fifth vital sign: exposing the vital need for pain education. Clin Ther. 2013;35(11):1728-32. DOI: 10.1016/j.clinthera.2013.10.001.
8. Campbell JN. APS 1995 Presidential address. Pain Forum. 1996;5(1):85-8. DOI: 10.1016/S1082-3174(96)80076-6.
9. Tynan MA, Polansky JR, Titus K, Atayeva R, Glantz SA. Tobacco use in top-grossing movies - United States, 2010-2016. MMWR Morb Mortal Wkly Rep. 2017;66:681-6. DOI: 10.15585/mmwr.mm6626a1.