Ancient vs. modern Medicine
In ancient medicine health was considered from a holistic perspective as the presence of equilibrium in the interaction between mind and body and among the different components or humors of the human organism. Disease came from the loss of this equilibrium, leading to an imbalance which should be cured in a process leading to the restoration of this functional equilibrium (1,2).
The lack of scientific knowledge at that time only allowed the use of basic therapeutic modalities based on empirical and sometimes esoteric paradigms by means of natural herbal products and surgical interventions that, generally, lacked scientific support. Accordingly, most of the recovery expectations lied in the natural healing capability of the body. In that sense, the French author and humanist, Voltaire, stated that “the art of medicine consists in amusing the patient while nature cures the disease” and in many clinical situations this was true.
With the progress of the scientific knowledge, especially from the XIX century, medicine and the rest of the health disciplines have undergone an extraordinary progress and improvement in the both the diagnostic and treatment modalities, with extraordinarily successful surgical and medico/pharmaceutical therapeutic options.
With this scientific progress we have been able to successfully control the majority of the most severe health problems of the society in the XIX and XX century as:
– Early infancy diseases (congenital, infectious).
– Respiratory infections (influenza, pneumonia, tuberculosis).
– Gastrointestinal infections.
– Cardiovascular diseases.
– Cancer.
Leading to a significant and quick rise in the life expectancy of the human population, at least in developed countries.
New challenges in Medicine
This prolongation of the life expectancy has also caused a significant shift of the age pyramid towards an aging population.
This situation has favored the emergence of “Non-Life Threatening but Long Lasting Diseases” (diabetes, arthritis, etc). These diseases, although present in ancient times, had a much lower prevalence due to the deadly consequences of the previously mentioned health hazards and the lack of diagnostic and therapeutic alternatives.
Psychoneuroendocrineimmune axis
Some of these “Non-Life Threatening but Long Lasting Diseases” share in common the fact of being the consequence of the loss of equilibrium of the PsychoNeuroImmune Axis or more precisely, the PsychoNeuroEndocrineImmune (PNEI) Axis (3). PNEI Axis, in a computing resemblance, is the Main Operating System of the body and contains the Primary Software Program that coordinates its most important functions, both somatic and psychoemotional. These Subsystems (Psychological, Neurological, Endocrine and Immune) form a complex network that integrates multiple input and output signals using afferent and efferent feedback to modulate the responses. This means that the PNEI Axis is an unstable, dynamic and constantly adapting system reacting to the external and internal stimuli that attempt to alter the homeostasis or functional equilibrium of the organism.
Psychoneuroimmunology (PNI) is the science that studies the PNEI Axis (4). This term was first introduced by Dr. Robert Ader during his presidential lecture to the American Psychosomatic Society in 1980. PNEI is the study of the interaction between psychological processes and the Nervous, Endocrine and Immune Systems of the human body. This concept has its historical origins in the papers of Dr. Hans Selye in the years 1950’s suggesting the existence of what he called the “GENERAL ADAPTATION SYNDROME” and showing the intimate relation between stress and the adrenal cortex as a protective system of overall health of the body. The alteration of this Adaptation System gives rise to what he called “ADAPTATION MALADIES” (5,6).
PNEI takes an interdisciplinary approach, incorporating and integrating all the health related disciplines whose contemporary advances have allowed a very significant growth of this field that will surely render significant outcomes in the future (7).
Hypothalamic-pituitary-adrenal axis and sympathetic nervous system
The brain and the immune system are the two major adaptive systems of the body and talk to each other through signaling pathways. The two major pathways that are involved in this cross-talk are the Hypothalamic-Pituitary-Adrenal (HPA) Axis, the primary stress management system of the body that responds to physical and mental challenges to maintain homeostasis, in part by controlling the body’s cortisol level, and the Sympathetic Nervous System (SNS). The activation of the SNS during an immune response might be aimed to localize the inflammatory response.
Dysregulation of the HPA Axis and accordingly, the PNEI Axis, leads to a “loss or alteration of health”, what Selye called “ADAPTATION MALADIES”.
To adequately understand this concept it is important to make a clear differentiation between two terms: DISEASE as a disorder of a structure or function that produces specific symptoms or affects a specific location and ILLNESS as a more comprehensive and integrative term that reflects a state of sickness affecting the body or mind. Actually, as defined by Cassell: “Illness is a subjective state of suffering (physical, psychological and social) and can only be understood and defined with reference to the sick individual” (8,9).
“Illnesses” share some common features:
– They are usually not deadly, although they produce significant functional limitation and, in many instances, pain. Nevertheless, some of the most severe forms may seriously threaten the patient’s life.
– Their etiology is still a subject of scientific debate and, in general, when textbooks describe these entities they explain that the etiology is unknown and probably due to the presence and interaction of a multifactorial pathophysiology that combines genetics, epigenetics, hormones, immunity, stress, nutrition, weather fluctuations, etc.
– They usually have a long lasting, persistent and fluctuating course, depending on the equilibrium of the PNEI Axis.
– They present frequent comorbidity with other illnesses related with the alteration of the PNEI Axis.
– In general there is an absence of valid and reliable diagnostic analytic and image methods to confirm the diagnosis that, consequently, will be mainly obtained from the anamnesis and physical examination.
– The limitation in the knowledge of the etiology of these illnesses leads to the impossibility of a definite curative treatment and, consequently, limits the therapeutic approach to symptomatic functional and pain alleviating modalities.
Central hypersensitivity syndromes
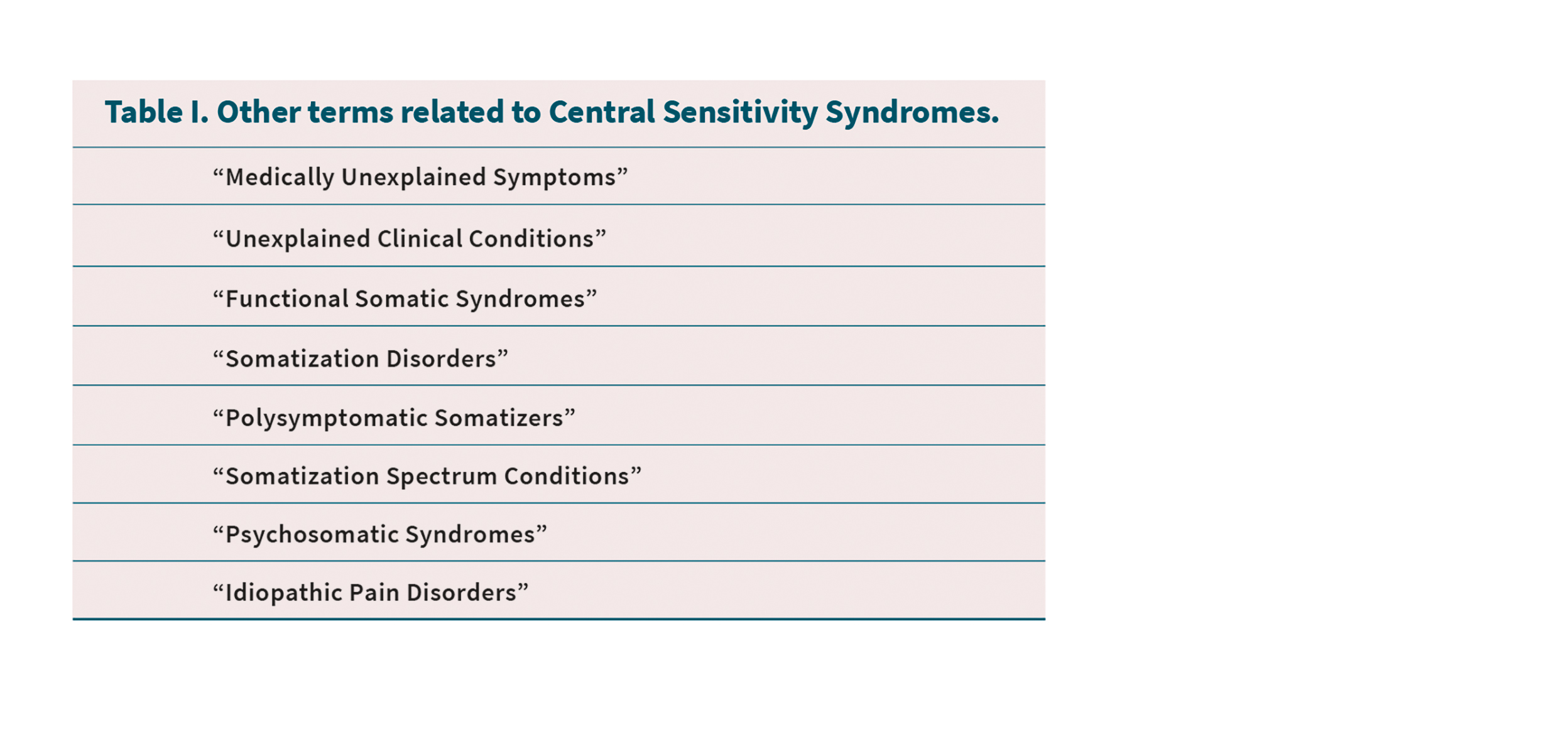
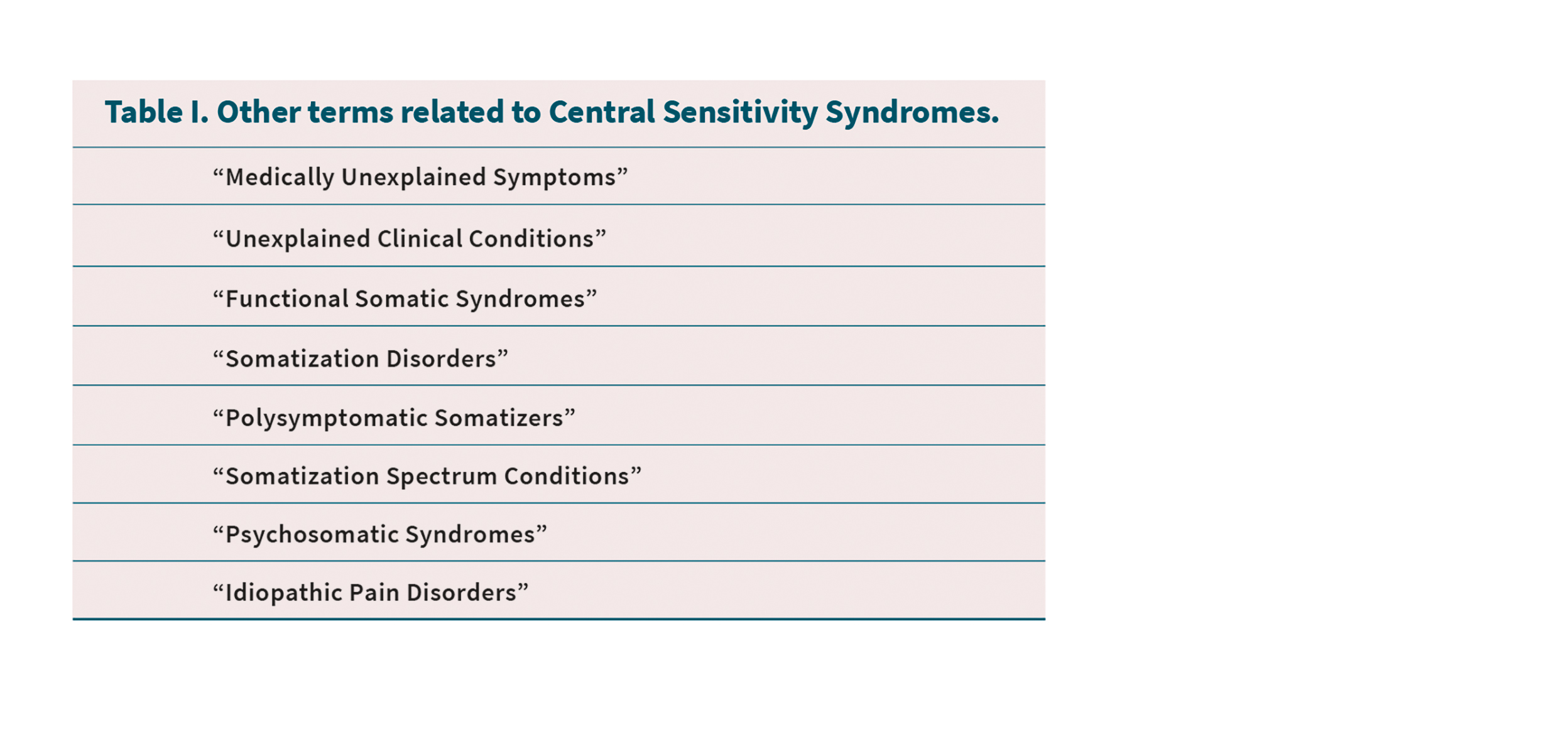
According to these concepts a new group of clinical entities has emerged in Medicine. Although there is still a debate regarding the terminology of these entities (Table I), it seems that they are going to be referred as CENTRAL HYPERSENSITIVITY SYNDROMES (CHSSs) (10). This confusion also affects at the understanding of the mechanisms underlying these clinical entities: some authors use the terms SENSITIZATION and SENSITIVITY interchangeably, but actually they refer to completely different concepts. SENSITIZATION is a secondary process in which the repeated administration of a stimulus results in the progressive amplification of the response both to this and other related stimuli. On the other hand, SENSITIVITY is a primary condition of a genetically related increased susceptibility of an organism to respond to external stimuli.
According to these terms, CHSSs could be defined as a collective term embracing a group of clinical problems that reflect the loss of equilibrium of the PsychoNeuroEndocrineImmune Axis in a genetically predisposed sensitive individual.
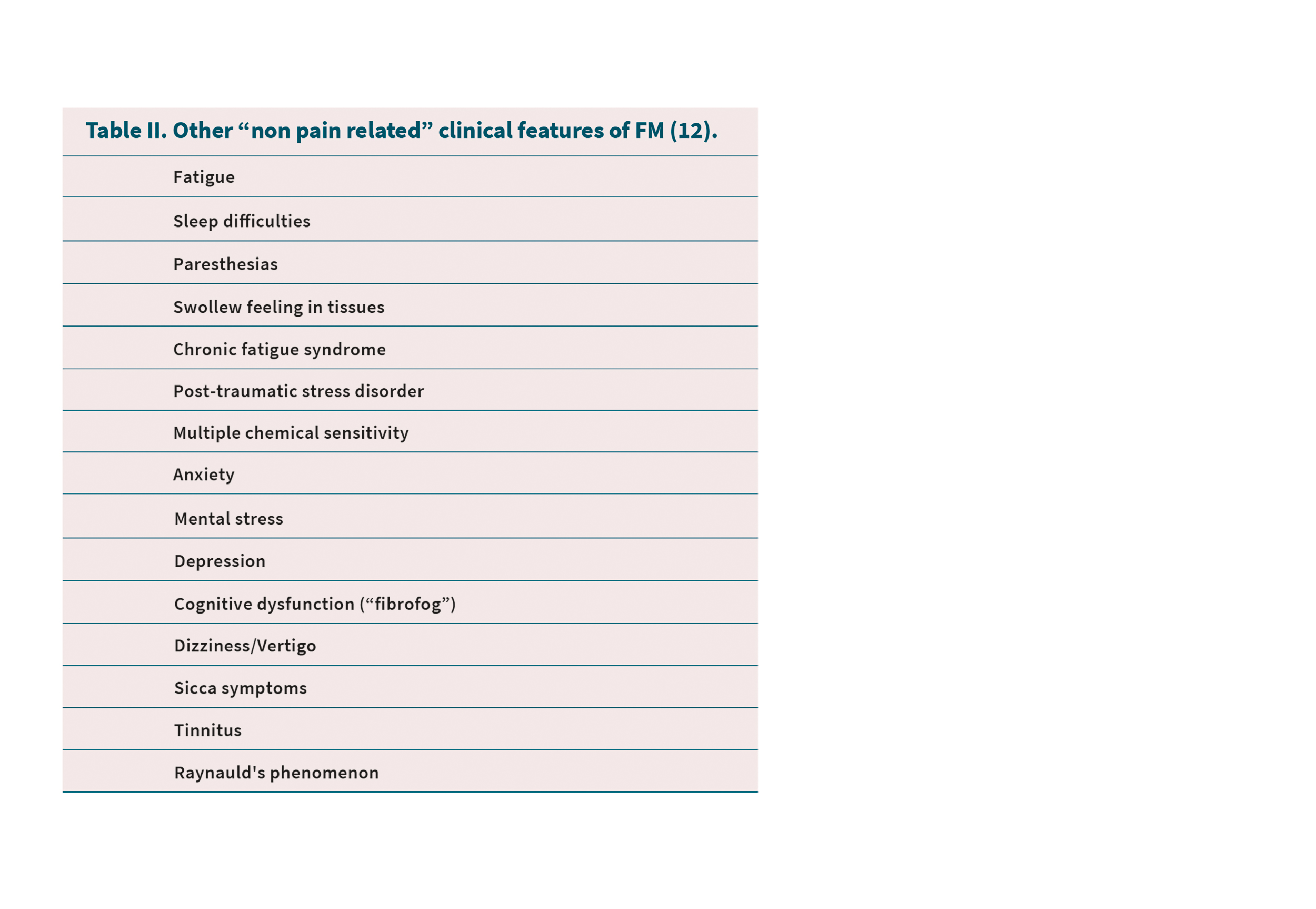
One of the first authors that proposed the existence of these entities was Dr. Yunus that highlighted the relation between Fibromyalgia (FM) and other Chronic Pain Conditions (11). Unfortunately, being pain one of the most significant symptoms of FM and these related chronic conditions, has led to confusion in the understanding of the fundamental pathophysiology that subsides under the CHSSs. In fact, FM presents other important clinical features besides widespread pain that cause significant functional limitation (Table II) (12). Certainly there are many clinical entities that can be included in the group of CHSSs that do not have pain as one of their main clinical manifestations. Almost all the systems in the body present, at least, a clinical entity that fulfils the criteria of CSS. Some of the most accepted are Fibromyalgia, Chronic Fatigue Syndrome, Irritable Bowel Syndrome, Multiple Chemical Sensitivity, Thyroid Gland Functional Disorders, Post-Traumatic Stress Disorder, Restless Legs Syndrome, Periodic Leg Movements Syndrome, Crohn’s Disease and Ulcerative Colitis but there are some others not fully accepted yet as Systemic Lupus Erythematosus, Scleroderma (Systemic Sclerosis), Dermatomyositis, Sjögren’s Syndrome, Polyarteritis Nodosa, Reiter’ Syndrome, Sweet Syndrome, Fernand Widal Syndrome, Asthma, Hay Fever, Idiopathic Labile Blood Pressure, Celiac Disease and Cyclic Neutropenia.
Some of the CSS dermatologic entities are Alopecia Areata, Chronic Urticaria, Eczema, Atopic Dermatitis, Raynauld’s Phenomenon, Vitiligo, Pityriasis Versicolor Psoriasis, Pemphigus and Pemphigoid.
In the female genitourinary system we have Premenstrual Syndrome, Female Urethral Syndrome, Interstitial Cistitis or Bladder Pain Syndrome (IC/BPS), Primary Dysmenorhea, Vulvodynia and Vulvar Vestibulitis.
It is important to emphasize the fact that not all subjects with a genetically predisposed hypersensitive PNEI Axis develop a CSS, the same way as not all the subjects with a psychopathological profile (obsessive, neurotic, depressive, etc) develop a psychiatric clinical condition. If that occurs, the integrative combination of the multifactorial pathophysiology (epigenetics, hormones, immunity, stress, nutrition, weather fluctuations, etc.) will condition that the clinical presentation of the CSS be to a certain point dependent more on the phenotypic architecture of the patient than on the genetic profile.
Orofacial central hypersensitivity
syndromes
The first reference to the subject of CHSSs in the Orofacial Area can probably be attributed to Dr. Dworkin who, in 1994, made a reference to this matter in the Journal of Prosthetic Dentistry with the question “Temporomandibular Disorders and Chronic Pain: Disease or Illness?” (13).
De Leeuw et al, in 2005, assessed whether certain medical conditions are more prevalent in female patients with orofacial pain than in age-matched controls. In the Results the authors show that the medical histories of subjects in the Orofacial Pain Group indicated a significantly greater number of medical conditions than did those of the subjects in the Control Group. Specifically, subjects in the Orofacial Pain Group reported having significantly more neurological, gastrointestinal, pulmonary, dermatologic and other conditions than did subjects in the Control Group. Subjects in the Orofacial Pain Group reported having 12 individual medical conditions significantly more often, than did subjects in the Control Group. The conclusion was that Orofacial Pain Patients seem to have more systemic comorbidities than normal subjects and that this fact may have therapeutic implications (14).
Burris et al, in 2010, examined the relationship between the medical comorbidities of patients with TMDs and their psychological functioning. The authors found that the mean total number of medical comorbidities of TMD patients was 3.49 and there was a linear relationship between the number of medical comorbidities and overall psychological distress (15).
In the Mouth, Face and Head, there are some entities that are already accepted as being part of the group of CHSSs as Masticatory Myofascial Pain, Tension Type Headache, Migraine, Atypical Odontalgia, Burning Mouth Syndrome, Idiopathic Dysgeusia (Phantom Taste) but, besides these ones, there are some other “Alterations of Health” that belong to this group as well:
– Geographic Tongue, an inflammatory condition of the mucous membrane of the tongue, usually on the dorsal surface. It is characterized by areas of smooth, red depapillation which migrate over time.
– Transient Lingual Papillitis that affects the fungiform papillae of the tongue.
– Recurrent Aphthous Estomatitis with repeated formation of ulcers in the mouth, in otherwise healthy individuals.
– Behçet Syndrome: Recurrent Oral Aphtous Ulcers, Genital Ulcers and Uveitis.
– Magic Syndrome: Mouth and Genital Ulcers with Inflamed Cartilage Syndrome.
– PFAPA Syndrome: Periodic Fever, Aphthous Stomatitis, Pharyngitis and Adenitis Syndrome.
– Lichen planus a disease of the skin and/or mucous membranes that resembles lichen. The most common clinical presentation is as a well-defined area of purple-coloured, itchy, flat-topped papules with interspersed lacy white lines (Wickham’s striae).
– Desquamative gingivitis, a descriptive term that refers to a red, shedding and ulcerated appearance of the gums.
– Oral Homogeneous Idiopathic Leukoplakia, a predominantly adherent white keratotic lesion of the oral mucosa that cannot be characterized as any other definable lesion.
– Oral Pemphigus and Pemphigoid.
– Recurrent Oral Herpes Simplex, a viral disease from the herpesviridae family caused by Herpes Simplex Virus type 1.
– Erythema multiforme, a skin condition of unknown cause, possibly mediated by deposition of immune complex (mostly IgM) in the superficial microvasculature of the skin and oral mucous membrane that usually follows an infection or drug exposure.
– Idiopathic Perioral Vitiligo, a condition that causes depigmentation of parts of the skin when melanocytes die or are unable to function.
– Oral Granulomatosis, a condition characterized by persistent enlargement of the soft tissues of the mouth, lips and the area around the mouth on the face that ocasionally presents together with Crohn’s Disease and Sarcoidosis.
– Melkersson-Rosenthal Syndrome, when Orofacial Granulomatosis occurs with fissured tongue and paralysis of the facial nerve.
– Linear Immunoglobulin A Dermatosis is an autoimmune subepidermal vesiculobullous disease that may be idiopathic or drug-induced.
Therapeutic considerations
When facing the therapeutic management of CHSSs usually the traditional “Biomedical Mechanistic” Model of Treatment based on the “cause and effect” concepts of the interventional Medicine have only a partial and frequently temporary effect, with recurrence of the symptomatology with occasional worsening presentation.
Without resigning to the symptomatic alleviation of the pain and functional limitation of the patient, the fundamental paradigm that must support the treatment of these pathologies must be based in the Biopsychosocial Model of therapeutic management proposed by Dr. Engel in 1970 (16). A close interaction among all the health care professionals involved is of mandatory importance in order to try to assist the organism to recover the equilibrium of the PNEI Axis. The multiple therapeutic modalities available from the Biological, Social and Psychological point of view must be employed in a coordinated and integrative manner. Unfortunately, we are still far from getting this interdisciplinary collaboration.
In these clinical entities related with primary Central Sensitivity the patient is an essential member of the therapeutic team. He or she must be instructed, in a sympathizing and affective dialogue, of the fundamental concepts that affect his/her malady. A detailed, comprehensive, though understandable, explanation of the delicate configuration of their PNEI Axis and its extraordinary capability to detect minimal modifications of the somatic and/or psychoemotional homeotasis leading to the initiation of, somehow, excessive and inadequate corrective actions of his/her body. They must understand the multifactorial etiology and pathophysiology of these illnesses and the therapeutic limitations of actual medicine. This reasoned understanding will surely have a positive effect, relieving the emotional distress and leading to the acceptance of the situation and the assertive commitment with the therapeutic protocol, something that will be very helpful in the recovery of the equilibrium of the PNEI Axis. In certain circumstances, this psychoemotional component of the therapeutic management will require a professional evaluation and treatment by a mental health specialist with the use of Acceptance and Commitment Therapy, an advanced modality of Cognitive Behavioral Therapy (17,18).
Conclusions
This paper, arising from a historical and holistic medical perspective, presents the concept of Central Sensitivity Syndromes as a group of clinical entities that reflect the loss of equilibrium of the PsychoNeuroEndocrineImmune Axis in a genetically predisposed sensitive individual.
In the orofacial area there are some entities that fulfill the criteria of CHSSs. A preliminary description of these pathologies is presented along with some therapeutic considerations regarding the need of a biopsychosocial multimodal interdisciplinary approach in which the patient plays an essential role in the long term management by means of understanding, acceptance and commitment.
REFERENCES
1. Schiefsky M. Hippocrates: On Ancient Medicine. Leiden: Brill Academic Pub; 2005.
2. Coulter HL: Divided Legacy: A History of the Schism in Medical Thought. The Patterns Emerge: Hippocrates to Paracelsus. Washington DC: Wehawken Book; 1975.
3. Tellez-Vilagra C, Beauroyre R. Eje PsicoNeuroEndocrinoInmunológico. Rev Esp Med Quir. 2002;7(2):5-14.
4. Irwin M, Vedhara K. Human PsychoNeuroImmunology. New York: Oxford University Press; 2005.
5. Selye H. The Stress of Life. New York: McGraw-Hill; 1956.
6. Selye H. Stress and disease. Science. 1956;122(3171):625-31. DOI: 10.1126/science.122.3171.625
7. Ader R, Cohen N. Behaviorally conditioned immunosuppression. Psychosom Med. 1975;37(4):333-40. DOI: 10.1097/00006842-197507000-00007.
8. Cassell EJ. The nature of suffering and the goals of medicine. New York: Oxford University Press; 1991.
9. Jennings D. The confusion between disease and illness in clinical medicine. CMAJ. 1986;135(8):865-70.
10. Yunus MB. Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Rheum. 2008;37(6):339-52. DOI: 10.1016/j.semarthrit.2007.09.003.
11. Yunus MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):339-56. DOI: 10.1016/j.semarthrit.2006.12.009.
12. Yunus MB. Role of central sensitization in symptoms beyond muscle pain, and the evaluation of a patient with widespread pain. Best Pract Res Clin Rheumatol. 2007;21(3):481-97. DOI: 10.1016/j.berh.2007.03.006.
13. Dworkin SF, Massoth DL. Temporomandibular disorders and chronic pain: disease or illness? J Prosthet Dent. 1994;72(1):29-38. DOI: 10.1016/0022-3913(94)90213-5.
14. de Leeuw R, Klasser GD, Albuquerque RJ. Are female patients with orofacial pain medically compromised? J Am Dent Assoc. 2005;136(4):459-68. DOI: 10.14219/jada.archive.2005.0201.
15. Burris JL, Evans DR, Carlson CR. Psychological correlates of medical comorbidities in patients with temporomandibular disorders. J Am Dent Assoc. 2010;141(1):22-31. DOI: 10.14219/jada.archive.2010.0017.
16. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129-36. DOI: 10.1126/science.847460.
17. Wetherell JL, Afari N, Rutledge T, Sorrell JT, Stoddard JA, Petkus AJ, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain. 2011;152(9):2098-107. DOI: 10.1016/j.pain.2011.05.016.
18. Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: a study of treatment effectiveness and process. J Consult Clin Psychol. 2008;76(3):397-407. DOI: 10.1037/0022-006X.76.3.397.